Stroke:无症状颈动脉狭窄患者进行CABG合并CEA术的5年结果
2022-09-11 MedSci原创 MedSci原创
在5年的随访中,与单独的CABG相比,尽管在统计上并不显著,联合CABG+CEA与较高的卒中或死亡比率有关。
尽管缺乏随机试验的证据,对于有冠状动脉疾病并伴有无症状的严重颈动脉狭窄的患者进行冠状动脉旁路移植术(CABG)和颈动脉内膜切除术(CEA)的联合治疗已被广泛采用。最近有研究表明,与单纯的CABG相比,CABG+CEA后30天内发生中风或死亡的风险更高。
近期,来自CABGCAS协作组织报告了CABG与无CEA后的长期结果。CABACS是一项随机、对照、多中心、公开的试验。接受CABG的无症状严重(≥70%)颈动脉狭窄患者被分配为CABG+CEA或单独CABG,随访时间为5年。主要次要终点包括非致命性中风或死亡,任何死亡和任何非致命性中风。
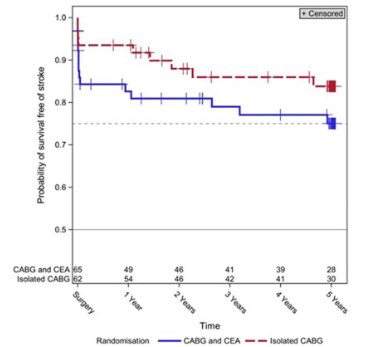
结果显示,5年后,各组之间的中风或死亡比率没有明显差异(CABG+CEA 40.6% [95% CI, 0.285-0.536],单独CABG 35.0% [95% CI, 0.231-0.484];P=0.58)。在CABG+CEA之后的任何时候,非致命性中风的发生率都较高(1年:19.3%对7.1%,P=0.09;5年:29.4%对18.8%,P=0.25)。两组5年内的全因死亡率相似(CABG+CEA:25.4%对单独CABG:23.3%,RR=1.148[95%CI,0.560-2.353];P=0.71)。亚组分析没有发现年龄、性别、术前改良的Rankin量表和中心对结果事件的任何明显影响。
在5年的随访中,与单独的CABG相比,尽管在统计上并不显著,联合CABG+CEA与较高的卒中或死亡比率有关。这主要是由于CABG+CEA后围手术期的风险不明显。
参考文献:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#颈动脉#
54
#无症状颈动脉狭窄#
48
#无症状#
37
#CEA#
37
#动脉狭窄#
37